Overview
What is ADHD?
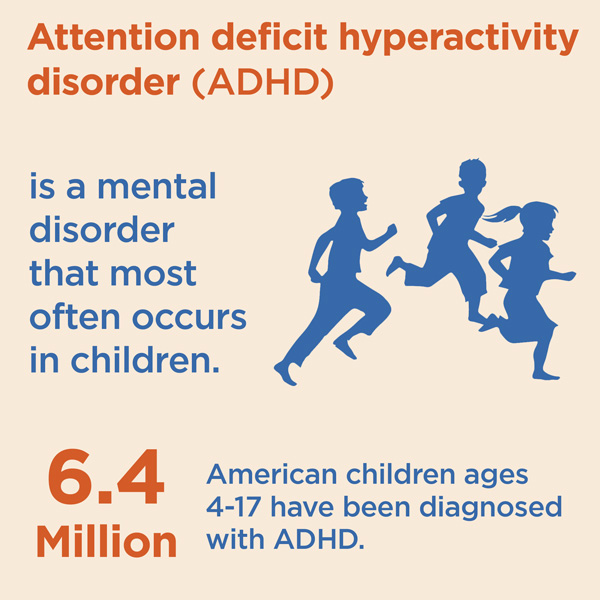
ADHD is a condition of the brain that makes it difficult for children to control their behavior. It is one of the most common chronic conditions of childhood. It affects 4% to 12% of school-aged children. About 3 times more boys than girls are diagnosed with ADHD.
Are there different types of ADHD?
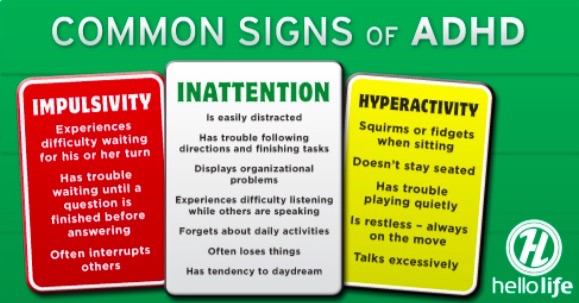
- Inattentive only (formerly known as attention-deficit disorder [ADD])— Children with this form of ADHD are not overly active. Because they do not disrupt the classroom or other activities, their symptoms may not be noticed. Among girls with ADHD, this form is most common.
- Hyperactive/Impulsive—Children with this type of ADHD show both hyperactive and impulsive behavior but can pay attention. They are the least common group and are frequently younger.
- Combined Inattentive/Hyperactive/Impulsive—Children with this type of ADHD show many symptoms in all 3 dimensions. This is the most common type of ADHD.
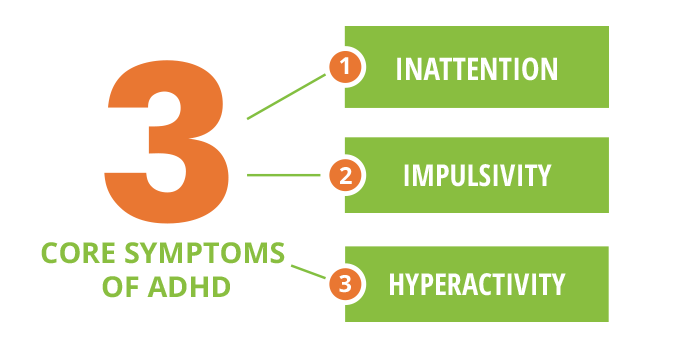
What are the symptoms of ADHD?
TABLE 1. Symptoms of ADHD
-
Inattention
- Often has a hard time paying attention, daydreams
- Often does not seem to listen
- Is easily distracted from work or play
- Often does not seem to care about details, makes careless mistakes
- Frequently does not follow through on instructions or finish tasks
- Is disorganized
- Frequently loses a lot of important things
- Often forgets things
- Frequently avoids doing things that require ongoing mental effort
-
Hyperactivity
- Is in constant motion, as if “driven by a motor”
- Cannot stay seated
- Frequently squirms and fidgets
- Talks too much
- Often runs, jumps, and climbs when this is not permitted
- Cannot play quietly
-
See your pediatrician for a Impulsivity
- Frequently acts and speaks without thinking
- May run into the street without looking for traffic first
- Frequently has trouble taking turns
- Cannot wait for things
- Often calls out answers before the question is complete
- Frequently interrupts others
How can I tell if my child has ADHD?
If your child has shown symptoms of ADHD for more than 6 months, discuss this with your pediatrician.
Diagnosis
A pediatrician will determine whether your child has ADHD using standard guidelines developed by the Indian Academy of Pediatrics.
There is no single test for ADHD. The process requires several steps and involves gathering a lot of information from multiple sources. You, your child, your child’s school, and other caregivers should be involved in assessing your child’s behavior.
To confirm a diagnosis of ADHD, symptoms must –
- Occur in more than one setting, such as home, school, and social situations and cause some impairment
- Significantly impair your child’s ability to function in some of the activities of daily life, such as schoolwork, relationships with family, and relationship with friends or in his ability to function in groups settings.
- Start before the child reaches 7 years of age but may be recognized later.
- Have continued for more than 6 months.
Pediatricians visit-
See your pediatrician for a complete physical and neurologic examination. He will need a full medical history to put your child’s behavior in context and screen for other conditions.
Your pediatrician may refer your child to a pediatric subspecialist.
- Mental retardation.
- Developmental disorder – Speech problems, motor problems, or a learning disability
- Chronic illness.
- Visual or hearing issues.
- Major anxiety, depression or aggression.
- Possible seizure disorder
- Possible sleep disorder
How will my child’s school be involved?
-
Teachers provide valuable insights. Your child’s teacher can discuss the following with your pediatrician:
- Your child’s behavior in the classroom.
- Your child’s learning patterns.
- How long the symptoms have been a problem.
- How the symptoms are affecting your child’s progress at school.
- Ways the classroom program is being adapted to help your child.
- Whether other conditions may be affecting the symptoms.
Coexisting conditions
Oppositional defiant disorder or conduct disorder
Up to 35% of children with ADHD also have oppositional defiant disorder or conduct disorder. These children tend to lose their temper easily, can annoy people on purpose & are defiant and hostile toward authority figures. They can break rules, destroy property, get suspended or expelled from school, and violate the rights of other people. These children are at much higher risk for getting into trouble with the law or having substance abuse problems than children who have only ADHD. This type of coexisting condition is more common among children with the primarily hyperactive/impulsive and combination types of ADHD.
Mood disorders/depression
About 18% of children with ADHD also have mood disorders such as depression or bipolar disorder (formerly called manic depression). There is frequently a family history of these types of disorders. Coexisting mood disorders may put children at higher risk for suicide, especially during the teenage years. These disorders are more common among children with inattentive and combined types of ADHD. Children with depression often require additional interventions or a different type of medication than those normally used to treat ADHD.
Anxiety disorders
These affect about 25% of children with ADHD. Children with anxiety disorders have extreme feelings of fear, worry, or panic that make it difficult to function. These disorders can produce physical symptoms such as racing pulse, sweating, diarrhea, and nausea. Counseling and/or different medication may be needed to treat these coexisting conditions.
Learning disabilities
Learning disabilities are conditions that make it difficult for a child to master specific skills such as reading or math. ADHD is not a learning disability. However, ADHD can make it hard for a child to do well in school. Diagnosing learning disabilities requires evaluations, such as IQ and academic achievement tests, and requires educational interventions.
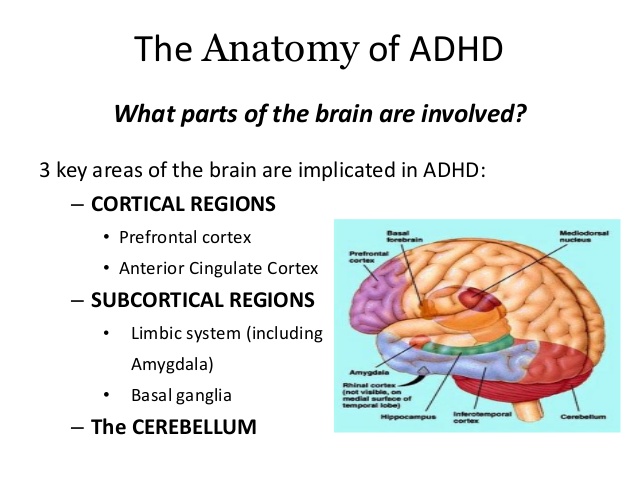
Causes of ADHD
ADHD is a biological disorder. A lower level of neurotransmitters in parts of the brain that control attention and activity level may be associated with ADHD. It can run in families.
It is the commonest comorbidity of epilepsy.
ADHD is often comorbid with other disabilities like hearing impairment, autism, ID etc.
Prematurity increases the risk of developing ADHD.
Are there any specific tests for ADHD?
Certain parent and teacher questionnaire can be used for defining the score of ADHD.
Management of ADHD
Management includes following steps
At the beginning of treatment, the doctor will set 3 to 6 goals for the child’s behavior. These target outcomes will guide the treatment plan. Your child’s goals outcomes should focus on helping her function as well as possible at home, at school, and in your community. You need to identify what behaviors are most preventing your child from success.
- Improved relationships with parents, siblings, teachers, and friends.
- Better schoolwork.
- More independence in self-care or homework.
- Improved self-esteem.
- Fewer disruptive behaviors.
- Safer behavior in the community.
The following are examples of goals:
- Realistic
- Achievable
- Measurable
The goals should be
- Follow-up activities
- Monitoring
- Education about ADHD – Educating the people involved about ADHD is a key part of treating your child. As a parent, you will need to learn about ADHD. Read about the condition and talk to people who understand it. This will help you manage the ways ADHD affects your child and your family on a day-to-day basis. It will also help your child learn to help himself.
- Teamwork among doctors, parents, teachers, caregivers, other health care professionals, and the child
- Medication
- Behavior therapy including parent training
- Individual and family counseling
Your child’s treatment plan will be set up to help her achieve these goals.
Treatment for ADHD uses the same principles that are used to treat other chronic conditions. Long-term planning is needed because these conditions are not cured. Families must manage them on an ongoing basis. In the case of ADHD, schools and other caregivers must also be involved in managing the condition.
These medications help children with ADHD focus their thoughts better and ignore distractions. This makes them more able to pay attention and control their behavior. Stimulants may be used alone or combined with behavior therapy. Studies show that about 80% of children with ADHD who are treated with stimulants improve a great deal once the right medication and dose are determined. Different types of stimulants are available, in short-acting (immediate- release), intermediate-acting, and extended-release forms. Immediate-release forms usually are taken every 4 hours, when the medication is needed. They are the cheapest of the medications. Intermediate-acting and extended-release medications usually are taken once in the morning.
Children who use extended-release forms of stimulants can avoid taking medication at school or after school. It is important not to chew or crush extended-release capsules or tablets. However, extended-release capsules that are made up of beads can be opened and sprinkled on food for children who have difficulties swallowing tablets or capsules.
- It may take some time to find the best medication, dosage, and schedule for your child.
- Your child may need to try different types of stimulants or other medication. Some children respond to one type of stimulant but not another.
- The amount of medication (dosage) that your child needs also may need to be adjusted. The dosage is not based solely on his weight. The medication schedule also may be adjusted depending on the target outcome. For example, if the goal is to get relief from symptoms mostly at school, your child may take the medication only on school days.
- It is important for your child to have regular medical checkups to monitor how well the medication is working and check for possible side effects.
Which medication is best for my child?
- Side effects occur sometimes. These tend to happen early in treatment and are usually mild and short-lived, but in rare cases can be prolonged or more severe. The most common side effects include
- Decreased appetite/weight loss
- Sleep problems
- Social withdrawal Some less common side effects include
- Rebound effect (increased activity or a bad mood as the medication wears off)
What side effects can stimulants cause?
Common medications
Generic class
- Methylphenidate, immediate-release
- Methylphenidate, intermediate-acting
- Methylphenidate, extended-release
- Amphetamine, immediate-release
- Amphetamine, intermediate-acting
- Amphetamine, extended-release
Stimulants
- Atomoxetine
Non-stimulant
- Significant increase in blood pressure or heart rate
- Growth delay
- Bizarre behaviors – The same sleep problems do not exist for atomoxetine, but initially it may make your child sleepy or upset her stomach. There have been very rare cases of atomoxetine needing to be stopped because it was causing liver damage.
- More than half of children who have tic disorders, such as Tourette syndrome, also have ADHD.
- Tourette syndrome is an inherited condition associated with frequent tics and unusual vocal sounds. The effect of stimulants on tics is not predictable, although most studies indicate that stimulants are safe for children with ADHD and tic disorders in most cases. Most side effects can be relieved by
- Changing the medication dosage
- Adjusting the schedule of medication
- Using a different stimulant or atomoxetine. Close contact with your pediatrician is required until you find the best medication and dose for your child. After that, periodic monitoring by your doctor is important to maintain the best effects.
- Stimulants and atomoxetine may not be an option for children who are taking certain other medications or who have some medical conditions such as congenital heart disease.
- Transient tics
Very rare side effects include
Most experts recommend using both medication and behavior therapy to treat ADHD. This is known as a multimodal treatment approach.
There are many forms of behavior therapy, but all have a common goal— to change the child’s physical and social environments to help the child improve his behavior.
Under this approach, parents, teachers, and other caregivers learn better ways to work with and relate to the child with ADHD. You will learn how to set and enforce rules, help your child understand what he needs to do, use discipline effectively, and encourage good behavior. Your child will learn better ways to control his behavior as a result. You will learn how to be more consistent.
Behavior therapy has 3 basic principles.
- Set specific goals. Set clear goals for your child, such as staying focused on homework for a certain time or sharing toys with friends.
- Provide rewards and consequences. Give your child a specified reward (positive reinforcement) every time she shows the desired behavior. Give your child a consequence (unwanted result or punishment) consistently when she fails to meet a goal.
- Keep using the rewards and consequences. Using the rewards and consequences consistently for a long time will shape your child’s behavior in a positive way.
Principles for behavior therapy
shows specific behavior therapy techniques that can be effective with children with ADHD.
| Technique | Description | Example |
|---|---|---|
| Positive reinforcement | Complementing and providing rewards or privileges in response to desired behavior. | Child completes an assignment and is permitted to play on the computer. |
| Time-out | Removing access to desired activity because of unwanted behavior. | Child hits sibling and, as a result, must sit for 5 minutes in the corner of the room. |
| Response cost | Withdrawing rewards or privileges because of unwanted behavior. | Child loses free-time privileges for not completing homework. |
| Token economy | Combining reward and consequence. Child earns rewards and privileges when performing desired behaviors. She loses the rewards and privileges because of unwanted behavior. | Child earns stars or points for completing assignments and loses stars for getting out of seat. The child cashes in the sum of her stars at the end of the week for a prize. |
- Keep your child on a daily schedule. Try to keep the time that your child wakes up, eats, bathes, leaves for school, and goes to sleep the same each day.
- Cut down on distractions. Loud music, computer games, and TV can be overstimulating to your child. Make it a rule to keep the TV or music off during mealtime and while your child is doing homework. Whenever possible, avoid taking your child to places that may be too stimulating, like busy shopping malls.
- Organize your house. If your child has specific and logical places to keep his schoolwork, toys, and clothes, he is less likely to lose them. Save a spot near the front door for his school backpack so he can grab it on the way out the door.
- Reward positive behavior. Offer kind words, hugs, or small prizes for reaching goals in a timely manner or good behavior. Praise and reward your child’s efforts to pay attention.
- Set small, reachable goals. Aim for slow progress rather than instant results. Be sure that your child understands that he can take small steps toward learning to control himself.
- Help your child stay “on task.” Use charts and checklists to track progress with homework or chores. Keep instructions brief. Offer frequent, friendly reminders.
- Limit choices. Help your child learn to make good decisions by giving him only 2 or 3 options at a time.
- Find activities at which your child can succeed. All children need to experience success to feel good about themselves.
- Use calm discipline. Use consequences such as time-out, removing the child from the situation or distraction. Sometimes it is best to simply ignore the behavior. Physical punishment, such as spanking or slapping, is not helpful. Discuss your child’s behavior with him when both of you are calm.
Behavior therapy recognizes the limits that having ADHD puts on a child. It focuses on how the important people and places in the child’s life can adapt to encourage good behavior and discourage unwanted behavior. It is different from play therapy or other therapies that focus mainly on the child and his emotions.
Tips for helping your child control his behavior
Parent training is available to help you learn more about ADHD and specific, positive ways to respond to ADHD-type behaviors. This will help your child improve. In many cases parenting classes with other parents will be sufficient, but with more challenging children, individual work with a counselor/coach may be needed.
Taking care of yourself also will help your child. Being the parent of a child with ADHD can be tiring and trying. It can test the limits of even the best parents. Parent training and support groups made up of other families who are dealing with ADHD can be a great source of help. Learn stress- management techniques to help you respond calmly to your child. Seek counseling if you feel overwhelmed or hopeless.
Ask your pediatrician to help you find parent training, counseling, and support groups in your community. Additional resources are listed at the end of this publication.
How can my child’s school help?

Your child’s school is a key partner in providing effective behavior therapy for your child. In fact, these principles work well in the classroom for most students. Classroom management techniques may include
- Keeping a set routine and schedule for activities
- Using a system of clear rewards and consequences, such as a point system or token economy (See Table 3.)
- Sending daily or weekly report cards or behavior charts to parents to inform them about the child’s progress
- Seating the child near the teacher
- Using small groups for activities
- Encouraging students to pause a moment before answering questions
- Keeping assignments short or breaking them into sections
- Close supervision with frequent, positive cues to stay on task Your child’s school should work with you and your pediatrician to develop strategies to assist your child in the classroom. When a child has ADHD that is severe enough to interfere with her ability to learn, 2 federal laws offer help. These laws require public schools to cover the costs of evaluating the educational needs of the affected child and providing the needed services. The laws are
- The Individuals with Disabilities Education Act, Part B (IDEA)
- Section 504 of the Rehabilitation Act of 1973 If your child has ADHD and a coexisting condition, she may need additional special services such as a classroom aide, private tutoring, special classroom settings or, in rare cases, a special school.
- It is important to remember that once diagnosed and treated, children with ADHD are more likely to achieve their goals in school.
Keeping the treatment plan on track
Ongoing monitoring of your child’s behavior and medications is required to find out if the treatment plan is working. Office visits, phone conversations, behavior checklists, written reports from teachers, and behavior report cards are common tools for following the child’s progress. Treatment plans for ADHD usually require long-term efforts on the part of families and schools. Medication schedules may be complex. Behavior therapies require education and patience. Sometimes it can be hard for everyone to stick with it. Your efforts play an important part in building a healthy future for your child.
Ask your pediatrician to help you find ways to keep your child’s treatment plan on track.
What if my child does not reach his target outcomes?
Most school-aged children with ADHD respond well when their treatment plan includes both medication and behavior therapy. If your child is not achieving his goals, your pediatrician will assess the following factors:
- Were the target outcomes realistic?
- Is more information needed about the child’s behavior?
- Is the diagnosis correct?
- Is another condition hindering treatment?
- Is the treatment plan being followed?
impulsivity. Children who are being treated successfully may still have trouble with their friends or schoolwork.
However, if your child clearly is not meeting his specific target outcomes, your pediatrician will need to reassess the treatment plan.
Teenagers with ADHD
The teenage years can be a special challenge. Academic and social demands increase. In some cases, symptoms may seem less severe as the child grows older but, in most cases, ADHD symptoms persist. According to the National Institute of Mental Health, about 80% of those who required medication for ADHD as children still need it as teenagers. Parents play an important role in helping teenagers become independent. Encourage your teenager to help herself with strategies such as
- Using a daily planner for assignments and appointments
- Making lists
- Keeping a routine
- Setting aside a quiet time and place to do homework
- Organizing storage for school supplies, clothes, CDs, sports equipment, etc
- Being safety conscious (eg, always wearing seat belts, using protective gear for sports)
- Talking about problems with someone you trust
- Getting enough sleep
- Understanding their increased risk of abusing substances such as tobacco and alcohol Activities such as sports, drama, and debate teams can be good places to channel excess energy and develop friendships. Find what your teenager does well and support her efforts to “go for it.” Milestones such as learning to drive and dating offer new freedom and risks. Parents must stay involved and set limits for safety. Your child’s ADHD increases her risk of incurring traffic violations and accidents.
It remains important for parents of teenagers to keep in touch with teachers and make sure that their teenager’s schoolwork is going well. Talk with your pediatrician if your teenager shows signs of severe problems such as depression, drug abuse, or gang-related activities.
Has the treatment failed?
While treatment for ADHD should improve your child’s behavior, it may not eliminate the symptoms of inattention, hyperactivity, and
Will there be a cure for ADHD soon?
While there are no signs of a cure currently, research is ongoing to learn more about the role of the brain in ADHD and the best ways to treat the disorder. Additional research is looking at the long-term outcomes for people with ADHD.
Frequently asked questions
Will my child outgrow ADHD?
ADHD continues into adulthood in most cases. However, by developing their strengths, structuring their environments, and using medication when needed, adults with ADHD can lead very productive lives. In some careers, having a high-energy behavior pattern can be an asset
Why do so many children have ADHD?
The number of children who are being treated for ADHD has risen. It is not clear whether more children have ADHD or more children are being diagnosed with ADHD. Also, more children with ADHD are being treated for a longer period. ADHD is now one of the most common and most studied conditions of childhood. Because of more awareness and better ways of diagnosing and treating this disorder, more children are being helped.
Are schools putting children on ADHD medication?
Teachers are often the first to notice behavior signs of possible ADHD. However, only physicians can prescribe medications to treat ADHD. The diagnosis of ADHD should follow a careful process.
